Managing Gelding Scars: Insights from Three Cases in My Practice
- Elisse Miki
- Apr 29, 2024
- 9 min read
Updated: May 26, 2025
Gelding scars are a common occurrence in horses that have been castrated. These scars can have an impact on pelvic functional biomechanics and are commonly a site of irritation.
In humans, when scar tissue forms in the pelvis, it can disrupt normal functioning of muscles and joints, leading to pain and limited mobility.
This type of dysfunction is a top priority in the human therapeutic realm so why not for our horses?
Scar tissue is easily one of the top five dysfunctions treated in my human practice. Working with post-surgical scar tissue is infact so well recognized in licensed human manual therapies that it is a requirement to learn for board examination in Canada.
How do Gelding Scars Form?
When the testicular cords and surrounding fascia are cut during castration, they can recoil upwards towards the abdominal cavity. Scar tissue forms as a result of the body's natural healing process in response to an injury or wound. When the skin, muscle, or other tissues are damaged, the cells at the site of injury release chemicals that trigger a cascade of events leading to the formation of scar tissue. This tissue is made up of collagen fibers that help to patch up the damaged area and prevent further injury.
Scar tissue is different from normal tissue as it lacks the same blood supply and nerve connections, which can lead to loss of function or sensation in the affected area.
Following castration, scar tissue and adhesions can form from the cut testicular cords and the surrounding fascia. This new scar, however, lacks mobility and vitality, in comparison to healthy tissue due to the reduction in blood flow. Resultantly, surrounding connective tissue (pelvic floor, abdominal wall, urogenitary organs) can become adhered causing more local inflammation and irritation.
While scar tissue forms as a natural response to injury and is an essential part of the body's healing process, it can lead to loss of function or sensation and pain in the area. Over time, as scar tissue solidifies this is when we may begin to see more widespread global affects of compensatory movement.
Neurological Components
In a 2019 study by Bengtsdotter et al., researchers identified neuromas—nerve tissue tumors associated with pain—on 21 spermatic cords from 20 dissected horses, with 8 cases exhibiting bilateral involvement [2]. Although the sample size was relatively small, these findings are noteworthy, suggesting the potential for broader neurological complications in equine health.
Current Research
Research in this area remains limited, but existing studies align with principles of human medicine.
A study published in the Journal of Equine Veterinary Science (2006) found that horses with gelding scars presented with altered biomechanics in the hind limbs [7]. Altered biomechanics can cause reductions in performance and predisposes the horse to increased risk of injury.
Two subsequent studies (2013, 2014) found that horses with gelding scars had higher levels of pain and discomfort compared to horses without scars [6] [4]. It was hypothesized that the presence of the scar tissue lead to the formation of adhesions, which are known to cause pain and discomfort.
Signs of gelding scar issues:
Unexplained lameness
Loss of hindquarter engagement
Loss of propulsion
Difficulty with canter transitions
Reduced flexbility in hindlimbs
Reduced flexibility in lower back
Bucking or kicking out during transitions
Disuniting
Aversive feedback on palpation of region
Cool to the touch sheath (if longstanding)
Heat/warmth/swelling around sheath (if inflammed)
Anatomy of the Spermatic Cord
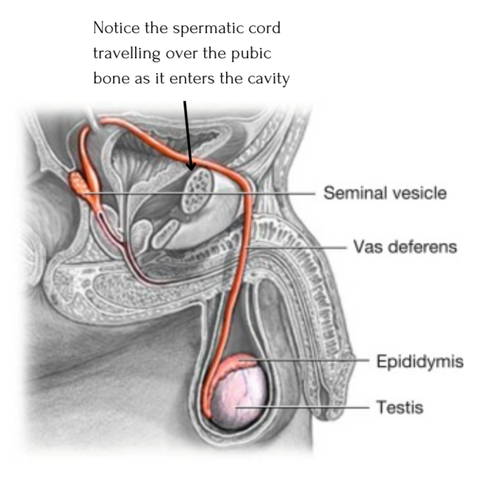
The spermatic cord travels from the testes through the superficial ring and then onto deep internal ring. The deep internal ring is located just above the midpoint of the inguinal ligament. If you are not familiar with the inguinal ligament this is a broad band of connective tissue which runs from pubic bone to ilium. This ligament alongside the transveralis fascia (which invaginates to form a covering of the contents of the inguinal canal) are what form the deep internal ring.
Human Anatomy
Highlighted here the key structures forming the superficial and deep inguinal ring, including the inguinal ligament (attaches from pubis to ilium). Plus a nice visual representation of the pathway for the spermatic cord. Remember the deep ring is bound by the inguinal ligament and the transversalis fascia. The spermatic cord is travelling through this ring of connective tissue!
Photo taken from https://pin.it/2fWIHGZVm
Equine Anatomy
In male horses, the deep internal ring may be palpated by locating external inguinal ring and the pubic bone at the top of the internal sheath.

Photo taken from https://pin.it/2fWIHGZVm
Why is Scar Tissue a Top Priority?
The pelvis is a complex structure that serves as the foundation for the horse's hindquarters. It is composed of several bones that are connected by joints and ligaments. The pelvic floor muscles play an important role in pelvic biomechanics, as they support the pelvic organs and help to control bladder and bowel function.
Gelding scars can affect pelvic biomechanics in several ways. They can cause adhesions to form between the pelvic bones and surrounding tissues. This can lead to a loss of flexibility in the pelvic area, which can affect the horse's movement and performance. Additionally, gelding scars can cause pain and discomfort, which can also affect the horse's movement, behavior, and quality of life.
A study published in the Journal of Equine Veterinary Science (2006) found that horses with gelding scars had altered biomechanics in their hind limbs [7]. It was ascertained that horses with gelding scars had decreased range of motion in the pelvic joints compared to horses without scars. The study also suggested that the decreased range of motion could potentially lead to lameness and a decrease in performance ability.
As discussed earlier, the presence of gelding scars can also lead to the formation of adhesions, which can cause pain and discomfort in the horse. Further research published in the Journal of Equine Veterinary Science (2014) found that horses with gelding scars had higher levels of pain and discomfort compared to horses without scars [6].
Three Cases From My Practice
In the videos below, you will see short clips from three cases worked with this past year. In each video you will see one of the range of motion test done for the SI joint and one gait evaluation video from the posterior view for each horse.
For privacy and confidentiality purposes, I am not able to share the full assessment process for each which always includes case history taking, observation (four views), gait evaluation (10 parameters), palpation (all affected structures), and range of motion testing (all joints).
Instead, with permission, I have selected two parameters that are able to most effectively demonstrate the immediate changes to range of motion and gait observed in each case while maintaining privacy and confidentiality.
As it relates to gelding scars, a range of motion test for the SI joint (alongside history, observation, palpation) and gait evaluation provide valuable evidence for indication to work with gelding scars and allows for re-evaluation immediately following intervention to determine efficacy.
As well paying close attention to the feedback from the horse is mandatory.
SI Joint Range of Motion Testing
In order to understand the videos you must first understand what is being evaluated. The SI joint is designed to move in various planes of motion on different axis. For this particular test we are assesing one of the primary axis of movement; mobility into inflare/outflare which in lay terms is outward movement and inward movement.
Consistent with principles of joint mechanics:

Normal physiology of the Hip-SI complex dictates approximation of the distal limb (focuses range of motion to the hip and SI joint) while bringing the limb into abduction creates outflare of the ilium. This should move easily without pain at least 30-45 deg with contribution from each of the hip and SI joint (using the hindlimb as a reference point). There should also be ability of lumbar spine and pelvis, as a whole, to transfer the load to the weightbearing side seen as a 'pelvic roll' or 'tilt' away from the tested side. This is good and considered normal.

Abnormal physiology may present as inability for the approximated limb to be taken into abduction creating outlfare of the ilium without onset of spasm, brace, bony block, pain and/or range of motion does not reach 30-45 deg. As well, a common sign of pelvic dysfunction is difficulty with load transfer through the lumbar spine and pelvis seen as lack of pelvic roll and/or rotation and what looks and feels like a "blocked" `movement at the level of the hip and SI joint (tuber sacrale region) as we bring the limb into abduction.
All videos were taken 60min apart following one treatment
Case #1
Case #2
Case #3
How Were These Results Obtained in1Hour?
Manual therapy. Soft tissue techqniues have been found to be effective in reducing the formation of scar tissue and improving tissue mobility in pre-existing scars.
One of the most effective manual therapy techniques for reducing scar tissue, in my experience, is myofascial release. Myofascial release involves the application of sustained pressure to the affected area to stretch and realign the fascia, which is the connective tissue that surrounds and supports all muscles and organs.
In a study published in the Journal of Bodywork and Movement Therapies (2017), researchers found that myofascial release was effective in reducing scar tissue and improving range of motion in patients with knee injuries [13].
Another effective manual therapy technique is frictions. Applying frictions involves the application of specific pressure in a longitudinal, cross fiber, or circular pattern to the affected area with the goal of evoking an inflammatory response which promotes healing and increased pliability. Current research indicates that frictions are effective in reducing scar tissue and improving function [14].
Both of these techniques alongside general osteopathic treatment techniques and isometric exercises were applied within the one hour session.
In Conclusion
Gelding scars can have a significant impact on pelvic functional biomechanics in horses. Adhesions and loss of flexibility in the pelvic area can affect movement and performance, while pain and discomfort can also have a negative impact on behavior. Certain manual therapy techniques may be effective in treatment and management while more complex cases may require surgery. Further research is needed to fully understand the anatomy of the pelvis in horses and the impact of scars on pelvic biomechanics. As always, it is important for horse owners to monitor their horse's behavior and movement patterns, and to seek veterinary care first if any issues arise.
Ready to Learn More?
Explore our Free Resources for tools you can use right away, dive into our Online Courses to deepen your knowledge, or join one of our Certification Programs to take your equine therapy practice to the next level.
References:
Afanador-Restrepo DF, Rodríguez-López C, Rivas-Campo Y, Baena-Marín M, Castellote-Caballero Y, Quesada-Ortiz R, Osuna-Pérez MC, Carcelén-Fraile MDC, Aibar-Almazán A. Effects of Myofascial Release Using Finding-Oriented Manual Therapy Combined with Foam Roller on Physical Performance in University Athletes. A Randomized Controlled Study. Int J Environ Res Public Health. 2023 Jan 12;20(2):1364.
Bengtsdotter EA, Ekman S, Andersen PH. Neuromas at the castration site in geldings. Acta Vet Scand. 2019 Sep 24;61(1):43.
Chen, W. Y., Abatangelo, G., & Greenspan, D. S. (2001). Wound healing and scar formation. In Mechanisms of fibrosis (pp. 275-308). Springer, Boston, MA.
Dalla Costa E, Minero M, Lebelt D, Stucke D, Canali E, Leach MC. (2014). Development of the Horse Grimace Scale (HGS) as a pain assessment tool in horses undergoing routine castration. PLoS One. 2014 Mar 19;9(3):e92281.
Eming, S. A., Krieg, T., & Davidson, J. M. (2007). Inflammation in wound repair: molecular and cellular mechanisms. Journal of Investigative Dermatology, 127(3), 514-525.
Freeman, K. P., & Ireland, J. L. (2013). The effect of castration on pain and discomfort in horses. Journal of Equine Veterinary Science, 33(12), 1089-1097.
Echte, A.-F., Schmidt-Ott, C., Claaßen, W., Heczko, K., Gremmes, C., & Gremmes, S. (2006). Lameness of horses caused by adhesion of the spermatic cord-a delayed complication of castration. Pferdeheilkunde Equine Medicine, 22(4), 445–448.
Gurtner, G. C., Werner, S., Barrandon, Y., & Longaker, M. T. (2008). Wound repair and regeneration. Nature, 453(7193), 314-321.
Lubczyńska, A., Garncarczyk, A., & Wcisło‐Dziadecka, D. (2023). Effectiveness of various methods of Manual Scar therapy. Skin Research and Technology, 29(3).
Maureen A Hardy, The Biology of Scar Formation, Physical Therapy, Volume 69, Issue 12, 1 December 1989, Pages 1014–1024.
Robert, M. P., Couturier, F., McGeown, P., Geffroy, O., & Tessier, C. (2020). Postcastration adhesions: Clinical signs, diagnosis, treatment and prognosis in 20 horses. Veterinary Record Case Reports, 8(4).
Searle, D., Dart, A., Dart, C., & Hodgson, D. (1999). Equine castration: Review of anatomy, approaches, techniques and complications in normal, cryptorchid and monorchid horses. Australian Veterinary Journal, 77(7), 428–434.
E Silva DCCM, de Andrade Alexandre DJ, Silva JG. (2017). Immediate effect of myofascial release on range of motion, pain and biceps and rectus femoris muscle activity after total knee replacement. J Bodyw Mov Ther. 2018 Oct;22(4):930-936.
Deflorin C, Hohenauer E, Stoop R, van Daele U, Clijsen R, Taeymans J. (2020). Physical Management of Scar Tissue: A Systematic Review and Meta-Analysis. J Altern Complement Med. 2020 Oct;26(10):854-865.
Barnes, M. F. (1997). The basic science of myofascial release: Morphologic change in connective tissue. Journal of Bodywork and Movement Therapies, 1(4), 231–238.